Pinworms
A young man came in about 3:00 in the morning worried he had overdosed on medicine for pinworms. He said he was standing in front of a convenience store when a passerby noticed him “itching my butt.” The other man told the patient he probably had pinworms. The other guy also said he just happened to have some pinworm medicine, which he offered to my patient. After taking one of the pills, my patient started getting worried he had overdosed, though he had no symptoms. He came to the emergency department and brought the pill bottle with him.
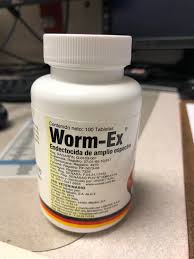
What he said he took was Worm-Ex. It is a broad-spectrum antiparasitic. This formulation was from Mexico and was specifically made for treating roosters used in cock fighting. Hence, the rooster logo on the nice yellow pill.* The bottle was clearly marked (in Spanish): For Veterinary Use.
The ingredients in the pill can also be used to treat parasitic infections in people so there was not a real worry about toxicity from taking medicine designed for animals. Also, the pills were for treating a rooster so you can rightly assume the dose was well below what one would prescribe to a human who needed to take the same medicine.
I explained to my patient that he had no reason to worry. The medicine was safe for humans to take and he took a very low dose. Though he had been unwise to take the medicine given to him by some guy in front of a convenience store, it was not dangerous and he need not worry at all about the consequences of his unwise decision.
This did not reassure him at all. He insisted that we pump his stomach as he was sure he was going to be poisoned. I questioned him some more as to why he was so worried. He insisted he had only taken one of these pills and nothing else. He assured me he had not wanted to hurt himself.
I tried all the logic I could think of to get him to see that, if he just took one of these pills, he had nothing to worry about. No matter what I said, he kept insisting that he was poisoned and needed his stomach pumped. By the time this went on for a while, I started to wonder if anything he was telling me was true. The idea that someone would see you itching your butt in front of a convenience store in the middle of the night, diagnose you with pin worms and just happen to have pinworm medicine to offer you just seemed too crazy to be true. But, was what really happened just as crazy? We will never know because he adamantly stuck to his original story and persistently refused to be reassured that he was not poisoned. He left a very unhappy patient with a very puzzled doctor.